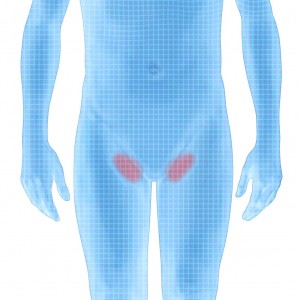
Inguinal or Groin Hernia
An inguinal hernia is a condition in which intra-abdominal fat or part of the small intestine, also called the small bowel, bulges through a weak area in the lower abdominal muscles. An inguinal hernia occurs in the groin—the area between the abdomen and thigh.
An inguinal hernia can occur any time from infancy to adulthood and is much more common in males than females.
Direct and indirect hernias are the two types of inguinal hernia, and they have different causes.
Symptoms of an inguinal hernia usually appear gradually and include a bulge in the groin, discomfort or sharp pain, a feeling of weakness or pressure in the groin, and a burning, gurgling, or aching feeling at the bulge.
An incarcerated inguinal hernia is a hernia that becomes stuck in the groin or scrotum and cannot be massaged back into the abdomen.
A strangulated hernia, in which the blood supply to the incarcerated small intestine is jeopardized, is a serious condition and requires immediate medical attention. Symptoms include extreme tenderness and redness in the area of the bulge, sudden pain that worsens quickly, fever, rapid heart rate, nausea, and vomiting.
An inguinal hernia is diagnosed through a physical examination.
Inguinal hernias may be repaired through surgery. Surgery is performed through one incision or with a laparoscope and several small incisions.
Surgery for inguinal hernia is usually done on an outpatient basis. Recovery time varies depending on the size of the hernia, the technique used, and the age and health of the patient.
Complications from inguinal hernia surgery are rare and can include general anesthesia complications, hernia recurrence, bleeding, wound infection, painful scar, and injury to internal organs

An abdominal wall hernia is a condition in which intra-abdominal fat or portions of the bowel bulges through a weak area in the lower abdominal muscles. An inguinal hernia occurs in the groin—the area between the abdomen and thigh. An inguinal hernia appears as a bulge on one or both sides of the groin. The bulge is more obvious when staining occurs. This type of hernia is called inguinal because fat or part of the intestine slides through a weak area called the inguinal canal. Blood vessels, nerves and the vas deferens traverse this canal traveling back and for the between the abdomen and the testicles. Compression of these structures by the hernia contribute they pain associated with this condition. An inguinal hernia can occur any time from infancy to adulthood and is much more common in males than females. Inguinal hernias tend to become larger with time.
The two types of inguinal hernia have different causes.
Indirect inguinal hernia. Indirect inguinal hernias are congenital hernias and are much more common in males than females because of the way males develop in the womb. In a male fetus, the spermatic cord and both testicles—starting from an intra-abdominal location—normally descend through the inguinal canal into the scrotum, the sac that holds the testicles. Sometimes the entrance of the inguinal canal at the inguinal ring does not close as it should just after birth, leaving a weakness in the abdominal wall. Fat or part of the small intestine slides through the weakness into the inguinal canal, causing a hernia. In females, an indirect inguinal hernia occurs in the same location as men but only the round ligament is traveling in the female inguinal canal so the pain pattern tends to be different.
Indirect hernias are the most common type of inguinal hernia. Premature infants are especially at risk for indirect inguinal hernias because there is less time for the inguinal canal to close.
In adults, inguinal hernias that enlarge, cause symptoms, or become incarcerated are treated surgically. In infants and children, inguinal hernias are always operated on to prevent incarceration from occurring. Surgery is usually done on an outpatient basis. Recovery time varies depending on the size of the hernia, the technique used, and the age and health of the patient.
Direct inguinal hernia. Direct inguinal hernias are caused by connective tissue degeneration of the abdominal muscles, which causes weakening of the muscles during the adult years. The hernia involves fat or the small intestine sliding through the weak muscles into the groin. A direct hernia develops gradually because of continuous stress on the muscles. One or more of the following factors can cause pressure on the abdominal muscles and may worsen the hernia:
sudden twists, pulls, or muscle strains
lifting heavy objects
straining on the toilet because of constipation
weight gain
chronic coughing
Indirect and direct inguinal hernias usually slide back and forth spontaneously through the inguinal canal and can often be moved back into the abdomen with gentle massage. Over time the tissues sliding back and forth may actually start to get stuck in the “out” position. This is called “incarceration” and typically presents as a bulge that never goes away. If bowel is involved in the incarceration it can occasionally become twisted or obstructed and this is considered a surgical emergency. Severe pain and vomiting are associated with this situation.
How is inguinal hernia diagnosed?
To diagnose inguinal hernia, the doctor takes a thorough medical history and conducts a physical examination. The person may be asked to stand and cough so the doctor can feel the hernia as it moves into the groin or scrotum. The doctor checks to see if the hernia can be gently massaged back into its proper position in the abdomen.
